Items filtered by date: December 2022
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Foot and Ankle Stress Fractures

Stress fractures are tiny, gradual bone cracks caused by overuse or repetitive activities, common in athletes. Unlike sudden regular fractures, they develop over time, often affecting the feet and lower limbs. Risk factors include excessive stress, hard surfaces, and rapid changes in exercise intensity. Other causes are weak muscles, joint issues, osteoporosis, medications, poor footwear, and vitamin deficiencies. Symptoms include localized pain, swelling, tenderness, and discomfort during high-impact activities. Diagnosis involves a physical assessment, potentially followed by an X-ray or MRI. Treatment includes rest, compression, training modification, and low-impact activities. Supportive footwear, custom foot orthotics, anti-inflammatories, and exercises can also help. Surgery may be needed in severe cases. Ignoring stress fractures can lead to complete fractures, non-healing, bone necrosis, and surgery. If you are experiencing foot or ankle pain, it is strongly suggested that you make an appointment with a podiatrist who can properly diagnose the issue and provide treatment options.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrists from Nola Sole Podiatry. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in New Orleans, LA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Are Bunions Affecting Your Everyday Life?
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
Caring for Diabetic Foot Wounds
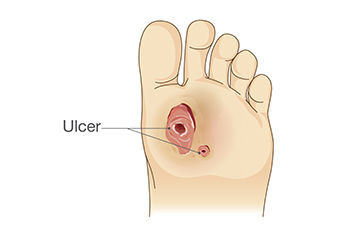
Managing diabetic foot wounds is important for individuals with diabetes, as they are susceptible to slow healing wounds that can escalate into severe complications. First, meticulous wound care is essential. This can begin with cleaning the wound daily with mild soap and warm water, followed by applying an antibiotic ointment and covering with a sterile dressing. Offloading pressure from the affected foot is suggested, as this can be achieved with special footwear, custom orthotics, or using assistive devices, such as crutches. Regular monitoring for signs of infection, such as increased redness, swelling, or discharge, is vital. Keeping blood sugar levels under control is fundamental, as high blood sugar can impede the healing process. If you have diabetes, it is strongly suggested that you are under the care of a podiatrist who can help you to manage any foot wounds that may develop.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Nola Sole Podiatry. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in New Orleans, LA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Handle a Long Work Day on Your Feet
In 2014, the American Podiatric Medical Association surveyed 1,000 American adults and found that half of all respondents lived with foot pain. Fortunately, there are ways to avoid foot problems such as following a daily footcare routine and wearing proper footwear at work.
If you have a job that requires you to be on your feet, it is best that you do not wear flat sole shoes. Your heel should be slightly elevated (less than 2 inches, but at least ¼-inch) if you are going to be standing for a prolonged period. You should also make sure that the shoes you wear are not too small. Tight shoes may cut off circulation to your feet, which will result in pain and blisters. It is always best to purchase fitted shoes later in the day, because the feet tend to swell as the day progresses. It may also be helpful to buy shoes a half size larger if you plan on wearing custom orthotics or arch supports.
Your muscles may become stiff when you are constantly standing up. It is important to take breaks every hour to stretch and relax. One tip is to perform calf raises, because this exercise will help improve your circulation. To perform this stretch, you first need to stand on the edge of a step with your abdominal muscles pulled inward. You then need to grip the step with the balls of your feet with your heels hanging over the edge. Next, try to raise your heels above the step by a few inches while standing on your tiptoes; hold this pose for a second. You should then lower your heels back even to the platform. These calf raises should be done ten times for full effectiveness.
You should also take care of your feet while you are at home. One of the best ways to prepare your feet for a long day of work is to soak them in ice water. Doing so for 20 minutes will help fight the swelling and inflammation that results from being on your feet at work.
Nevertheless, if you are experiencing pain in your feet, you should seek help from your podiatrist. Your doctor will help treat any ailments you may have in addition to helping you prevent any other ailments from developing in the future.
Protecting Your Feet While Standing at Work

For many, a typical workday involves prolonged periods of standing, which can take a toll on your feet, if not managed properly. There are essential tips to help you protect your feet while standing at work. Invest in supportive footwear This can begin by choosing shoes that provide adequate arch support and cushioning, and brands designed for all-day comfort. Using anti-fatigue mats can help reduce the strain on your feet and legs. Additionally, it can be beneficial to change your stance. This can be done by shifting your weight from one foot to the other or by taking small steps to avoid placing constant pressure on a single area. Some people find it helpful to wear compression stockings which can improve blood circulation in your legs and reduce swelling. Whenever possible, sit down or elevate your feet during breaks to relieve pressure and improve circulation. Performing simple foot and leg stretches during breaks can help to keep your muscles engaged and prevent stiffness. Excess weight can exacerbate foot discomfort, so maintaining a healthy weight can alleviate some of the strain on your feet. If you would like more information about foot protection while standing at work, it is suggested that you consult a podiatrist for additional useful tips.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact one of our podiatrists from Nola Sole Podiatry. Our doctors will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in New Orleans, LA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Facts About Morton’s Neuroma
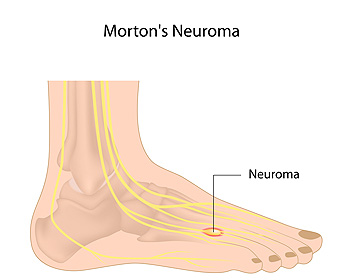
Morton's neuroma is a relatively common but often misunderstood foot condition that can lead to discomfort and pain. This condition can be demystified by exploring essential facts about Morton's neuroma. Morton's neuroma typically occurs between the third and fourth toes, though it can develop in other spaces in the foot. Despite its name, Morton's neuroma is not a tumor. It is actually a thickening of the tissue surrounding the nerves leading to the toes. Common symptoms can include sharp, burning pain or the sensation of a pebble in the shoe, typically while walking or running. Morton’s neuroma can be triggered by wearing tight shoes, high heels, or activities that put repetitive pressure on the forefoot, such as running. Treatment of Morton's neuroma can be managed with conservative measures such as wearing wider shoes, or using cushioned insoles. If conservative treatments do not provide relief, surgical removal of the neuroma may be considered. Effective preventive measures include wearing proper footwear, maintaining a healthy weight, and addressing foot issues promptly. If you have any of these symptoms, it is suggested that you consult a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact one of our podiatrists of Nola Sole Podiatry. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in New Orleans, LA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Choosing the Right Running Shoe
Choosing the right running shoes for you is an important part of running. A good pair of running shoes will make the running experience more enjoyable for you and prevent potential injury.
Poorly-fitted shoes can increase the risk of injury in runners substantially. Common injuries from running with poor quality shoes include shin splints, sprained ankles, Achilles tendinitis, stress fractures, plantar fasciitis and more. This is due to the fact that bad shoes do not provide proper foot support, can increase pronation (how much the foot rolls when hitting the ground), have little to no cushioning, do not allow the feet to breath, and do not provide enough flex and rigidity in the right parts.
When looking for running shoes, first, determine where you will be running. If you are a trail runner, then pick trail shoes. If you run on concrete and asphalt, then regular running shoes are the best choice. When trying on shoes, its best to go at the end of the day as feet grow during the day and shrink after a night of sleep. Shoes should be more rigid towards the back of the foot while being more flexible up where the toes are. The toe box should provide enough room for the toes to move freely. The overall fit should be snug, not too tight but not too loose. A good pair of running shoes should also provide enough arch support for your foot type. If you experience overpronation or under-pronation while running, try to find a pair of shoes that will help correct this with different sole patterns. Finally, try to find a pair of shoes that allow the feet to breathe like nylon mesh or synthetic leather.
Don’t forget about the socks either. Socks that hold too much moisture can lead to athlete’s foot. Socks should be breathable so that your feet can air out and breathe. Synthetic socks wick away moisture like sweat. If you tend to run a lot, having a second pair of shoes that you can wear while you let the first pair air out is smart. Just don’t forget to replace your shoes after about every 300 to 500 miles.
Before you start running, it is advised to see a podiatrist to see if running is right for you. They can also offer good advice on how to run and what to look for in a pair of running shoes. If you have flat feet or poorly supported ones, they can also offer custom-made orthotics that will help give your feet the support they need.

